Nearly 3,600 patients living with dementia, amyotrophic lateral sclerosis (ALS) and other neurological conditions will be supported annually by the year 2030, thanks to a new $6.6 million initiative by the National Neuroscience Institute (NNI) and the Lien Foundation.
As part of the programme – aptly dubbed NeuroPal – palliative care will be integrated earlier into a patient’s care journey, beginning with coordinated discussions across a multidisciplinary team of psychologists, occupational therapists, speech therapists and medical social workers, among others.
Neurological disease is a cruel thief that steals your thoughts and memories. It sneaks into your home, rearranges your furniture when you’re sleeping and leaves you terrified.
Lee Poh Wah, CEO of the non-profit Lien Foundation, says,
Rather than waiting until the end of life to administer palliative care, he says that incorporating it earlier into the care process helps relieve symptoms and the stress of the neurological disease. It also eases the burden of caregivers, who often have to spend “years” caring for people progressing through the stages of serious neurodegenerative disease.
NeuroPal represents a paradigm shift in how we care for patients with dementia, Parkinson’s disease, ALS and other neurodegenerative conditions seen at NNI.
Associate Professor David Low, Deputy Chief Executive Officer (Clinical) and Senior Consultant, Neurosurgery at NNI, says,
"By integrating palliative care principles early in our patients’ care journey, we can provide appropriate support and medical care to relive symptoms and enable patients to focus on what matters most to them."
In Singapore, palliative care is often provided only at the very end of a person’s journey, with a disproportionate focus on cancer patients. The average duration of care for non-cancer patients clocks in at around just nine days, compared to cancer patients’ 33.
Advertisement
Compare this to a patient’s journey with neurodegenerative disease, which can last years, if not decades.
It is also wrongly characterised as pain management, when in fact it means any form of care that improves quality of life.
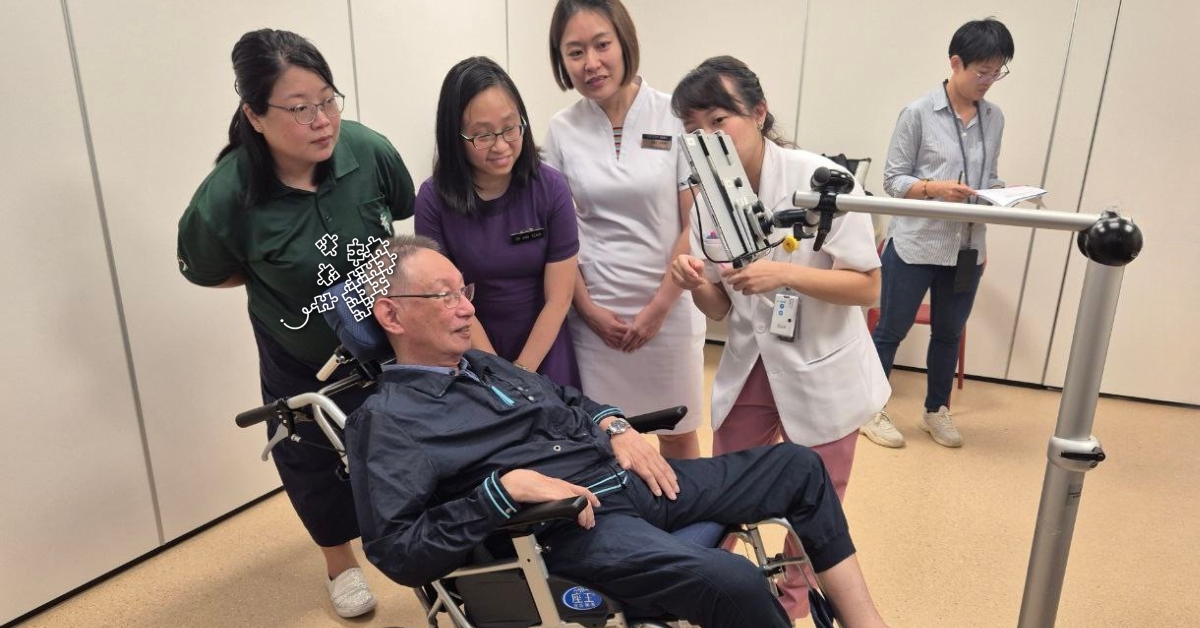
Take 71-year-old Chia Shyh Shen, who was diagnosed with ALS in 2022, for example. Before losing most of his mobility below the neck, he worked with a physiotherapist and occupational therapist to adjust to his changing body.
Though he enjoyed gardening in his backyard, he gradually shifted to working with small terrariums. More recently, he’s been working with a Tobii eye tracking device which allows him to navigate YouTube and play games without the help of a caregiver.

Almost 2,000 people benefited since April 2024
NeuroPal has been rolled out at clinics in Tan Tock Seng Hospital since April 2024, and more recently at Singapore General Hospital.
More than 1,850 patients have already been screened to date, with about one in five of those identified as requiring specialised neuro-palliative or supportive intervention.
The screening involves a short, simple questionnaire assessing patients’ symptoms and difficulties, with the goal of better informing doctors ahead of schedule appointments. These surveys also serve to help physicians adjust support according to patients’ evolving needs.
For example, a patient might be referred to an occupational therapist if they report facing difficulties with putting on clothes.
Though such referrals were already happening before the initiative was put in place, Associate Professor Adeline Ang, Senior Consultant, Neurology at NNI and co-lead of the NeuroPal programme, explains that the initiative represents “a mindset shift towards a more holistic approach to care”.
Rather than relying on the discretion of individual doctors, there is now “protected time” for “formalised discussions” among the hospital’s multidisciplinary team, says Dr Ang Kexin, Senior Consultant, Neurology at NNI.
Progressive training courses for wider neuro-palliative care ecosystem
In the longer term, the NeuroPal initiative will also see the development of neuro-palliative care for the wider healthcare ecosystem, both at NNI and beyond.
This ensures that any healthcare professional – not just palliative care specialists – will be able to “do their highest duty and minimise suffering”, says Lien Foundation’s Poh Wah.
Training courses will be rolled out progressively over the next two years. These include an online course for community care partners, allied healthcare professionals and general practitioners, as well as a comprehensive training course for supporting patients with neurodegenerative diseases for NNI doctors, nurses and clinical psychologists.
Partnerships between hospital and community hospices will also be strengthened to improve patient access to care facilities.
NeuroPal is the second initiative centred around palliative care to be unveiled by the Lien Foundation this year. Earlier, they announced a partnership with the National Heart Centre called Heartlanders, which aims to help some 9,000 heart failure patients over the next five years.