
A lot of us think and talk about eating healthy these days, but do we really know what ‘healthy’ looks like on a plate or in a cup? Enter the continuous glucose monitor or CGM.
Along with a fellow bunch of health coaches, I’ve been tracking my glucose levels with this nifty bit of tech. It’s like monitoring daily step counts or tracking sleep with a watch or ring.
A CGM is a small device worn stuck on your arm, usually for two weeks. It tracks glucose in the fluid between cells, aka interstitial fluid. This is a delayed proxy for blood glucose measurements. While it takes 5-20 minutes for blood glucose levels to be reflected in interstitial fluid, it does give a pretty good idea of how your body is responding to what you ate.
This information is beamed over Bluetooth and shows up on an app on your smartphone. Continuous means you get to see how your blood sugar rises and falls over 24 hours, unlike the ‘snapshots’ given by a finger prick blood glucose test.
Think video vs photos. Which tells a more complete and compelling story?
Advertisement
Know thyself through glucose monitoring

Image courtesy of Kim Lee
I like tech, and I like understanding my body — especially as it changes over the years. I know I can’t keep eating the same way I did in my 20s, and not pay for it in my 60s. Does anyone else relate to that?
So I tried a CGM early this year.
To be clear, a CGM is a medical device usually meant for Type 1 and Type 2 diabetics. It debuted in 1999. Since then, legions of non-diabetic, health-conscious individuals all over the world have latched on to its potential for showing them how they can customise diets and lifestyles to improve and optimise health.
CGM stories across social media come from everyday Joes to celebrity biohackers, athletes and even medical doctors.
They’re worn for a host of reasons, like research, to optimise weight management, insights into metabolic health, improve energy levels, mental clarity, aid food strategies for performance and recovery, etc.
How can wearing a CGM help in these cases?
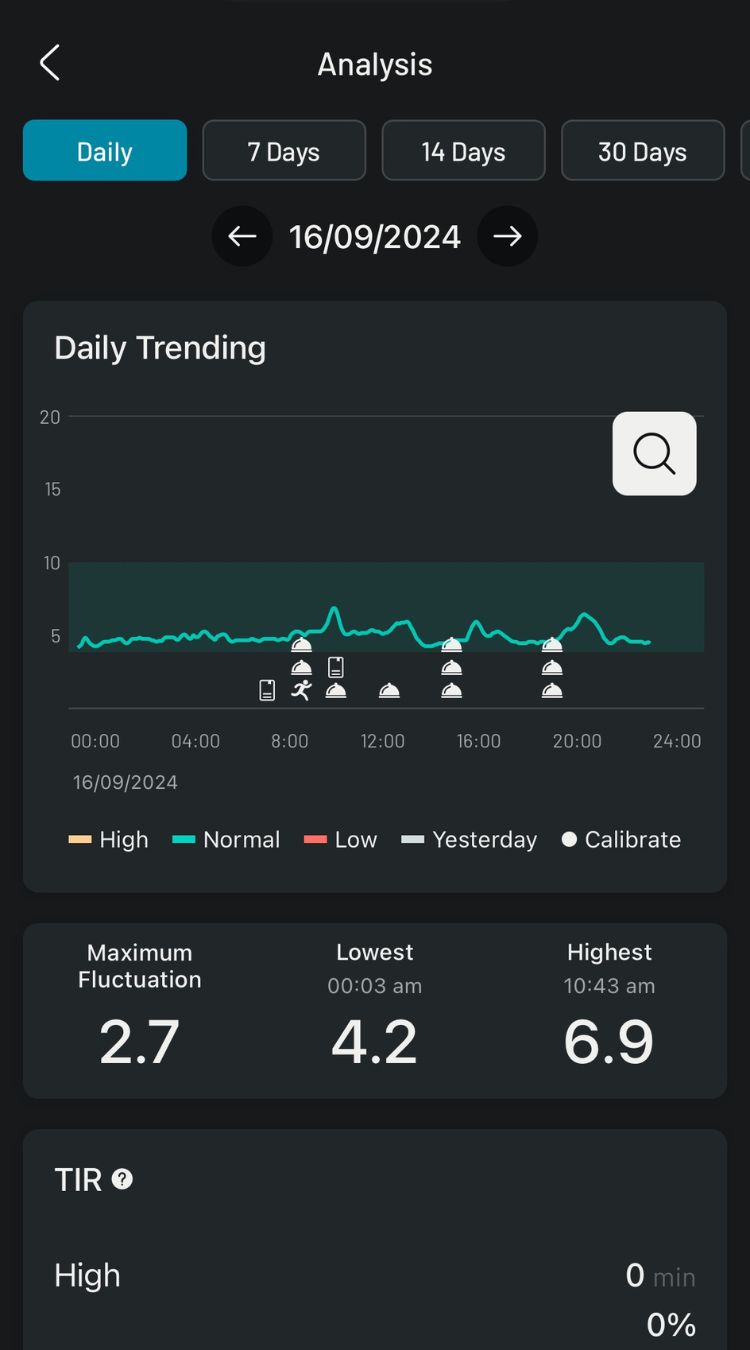
Image courtesy of Kim Lee
One of the rules of healthy eating (and drinking) is to not cause a sharp rise, or spike, your blood sugar — at least, not too often. And if that reading does spike, as it so often will from the carb-rich offerings in our urban foodscape, it should return close to your pre-meal blood sugar level before your next meal.
Otherwise, we are setting ourselves up for diabetes or likely other chronic health and metabolic issues. These problems can take decades in the making, one glucose spike at a time…
What’s so bad about high blood glucose levels?
Beyond the blood sugar sweet spot
The sweet spot for us is just 4 grams of glucose per litre of blood. More than that can fire up inflammation, organ and cell damage. Any less, and we may feel shaky, dizzy, confused, disoriented or worse.
Insulin is the hormone that keeps us at this safe level. Too much glucose in the blood? It shows up to rescue the situation by moving glucose out of blood and into the cells. Frequently spiking or chronically elevated blood glucose damages our sensitivity to insulin.
Insulin sensitivity runs on a continuum,
explains Dr WK Lam, a physician at 1doc i-Wellness Clinic Novena.
"By the time you are diagnosed diabetic by current diagnostic criteria, you would have had a few years of deteriorating metabolic health, and worsening insulin sensitivity."
This less-than-optimal blood sugar metabolism plays a part in “death and debility arising from common causes of death like cancers, arteriosclerosis, neurodegenerative diseases and metabolic diseases,” says Dr Lam.
The War Within
Even before things get that grim, observant people would have noticed how sugar-laden foods that cause blood glucose fluctuations can make them cranky, moody, even anxious.
On top of that, a poor diet often saps our motivation to exercise, or even move.
Poor metabolic health stems from suboptimal diet choices, and inadequate activity levels,
explains Dr Lam.
Other things associated with blood sugar swings are energy highs, lethargy, cravings for a sugary or unhealthy ‘fix’, bloating, and even poor sleep.
In everyday living however, we’re generally unaware of what our blood glucose levels are doing. And so, most of us make less than optimal choices for food and drink. Daily. Often several times a day. This adds up.
To make it more complicated, everyone’s body responds differently, even to the same food. Age, sex, whether one is a jock or a couch potato, stressed or relaxed, on medication/s (or not), pregnant, menopausal, even time of day, and more, can affect response. The information is unique to each individual.
What if there was a way to know and navigate this invisible threat? And it is with this question that I tried a CGM.
CGM glucose monitoring results
Here are some things I discovered in my two weeks with a CGM.
- Same meal, different Outcomes
I ate an open-face sourdough salmon and cream cheese sandwich loaded with avocado and sprouts on two different days.
Results: When I got up after eating to clean the house, my blood sugar level played nice, rising gently within the healthy range indicated by a shaded band on my app. But it shot up when I laid back to binge videos after dining.
I now see the wisdom of a post-prandial walk.
- What looks healthy isn’t necessarily so
I thought I was clever turning takeaway chicken rice into a healthier salad. I do this by shredding the steamed chicken, adding half a densely packed box of salad leaves, extra sliced cucumber and tomatoes, a 1/4 diced avocado, and just a third of the portion of rice. I toss the lot with a drizzle of olive oil and juice of half a lime.
Result: Blood sugar spiked out of range, likely because of the rice. I’ve noticed since then that white rice is not nice for me.
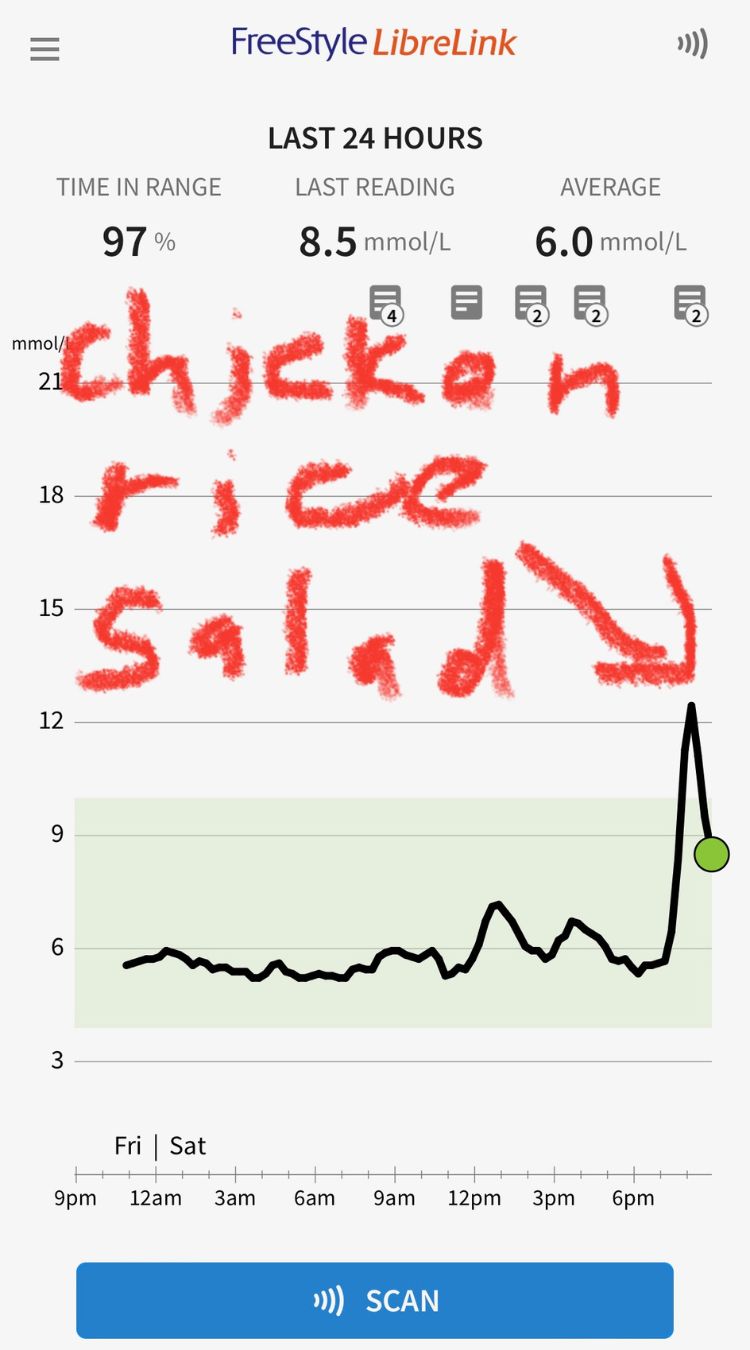
Image courtesy of Kim Lee
- Poor choices add up
Mooncake and durians! Friends shared homemade mooncakes at brunch after a 2-hour workout together, and I ate a rice-free bibimbap to make room for the sweet mooncake. This meal was followed by a later-than-usual dinner (8pm) with durian for dessert.

Image courtesy of Kim Lee
Result: In spite of the exercise and skipping rice to dampen glucose response, the quarter of a smaller-than-usual mooncake spiked to my highest blood sugar reading on the sensor.
It also gave me a head buzz that intensified into a mild headache for the next two hours. Sugar is not my friend!
The durian dessert after dinner also sent my blood sugar almost as high as the little piece of mooncake did.
And, horrors! Instead of falling at night like it usually does, my glucose readings stayed significantly higher than usual, digesting slowly as I attempted to sleep. Yes, it made for a night of restless and unsatisfying sleep!😫
- Poor sleep, higher numbers
I usually average seven hours of sleep. But after a couple of nights of restless and inadequate sleep, my blood sugar numbers rose higher than usual, so I really had to be careful what I ate to stay within range the following day.
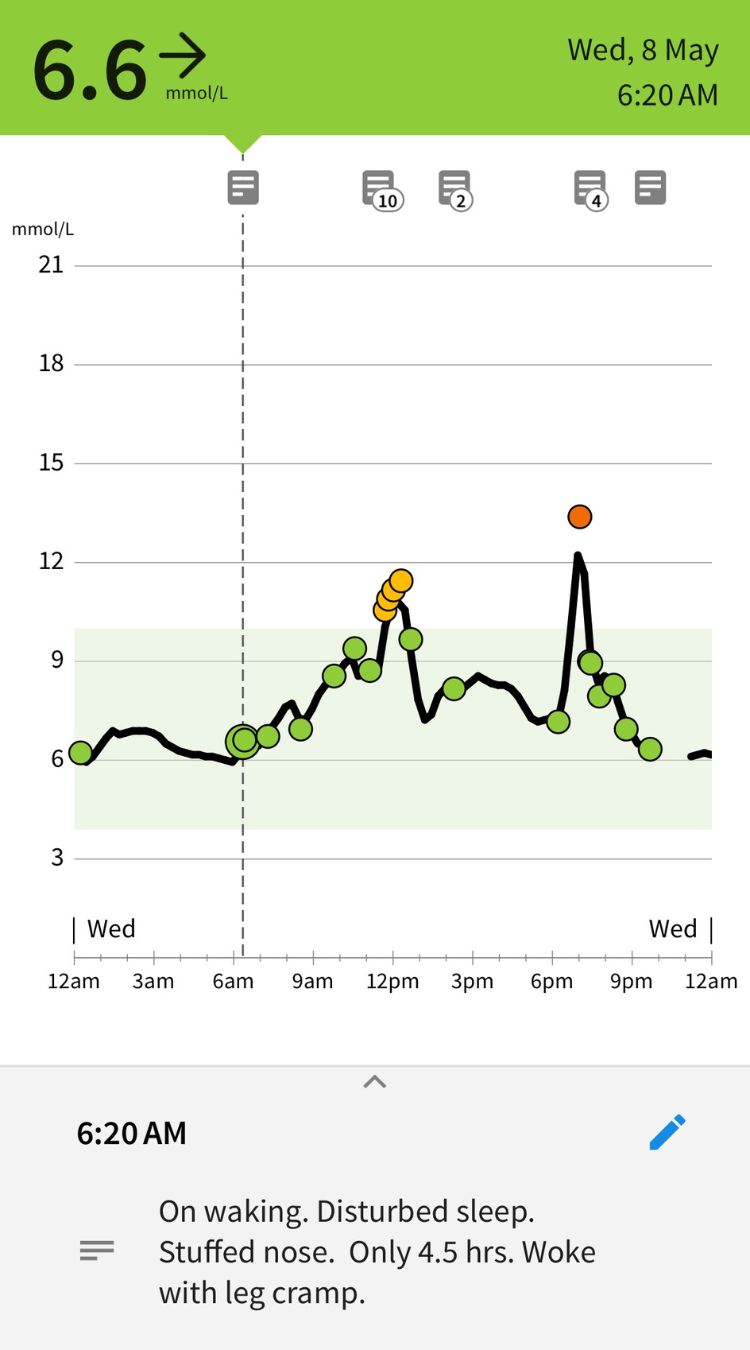
Image courtesy of Kim Lee
- What Works (for me)
What helps keep my blood glucose playing nice within range are:

Image courtesy of Kim Lee
- Creating meals focused on whole, fresh foods, with adequate protein for my level of activity, and generous helpings of vegetables, with whole grains, if any at all.
- Water – it’s calorie free!
- Finishing dinner by sunset, and getting at least 7 hours of sleep
- Moving briskly after eating, especially a big meal
- Doing big meals earlier in the day
- Opting for proteins and veg whenever possible when eating out
- No dessert with dinner, unless it’s a sensible portion of fruit, i.e. half a cup.
Reflections on wearing a CGM glucose monitor
Being able to see my glucose response became like a game to eat in a way that keeps glucose levels steady within the target zone. It made me think of a video driving game – staying in the target zone was like staying on the road.
If you’re still reading this and thinking of trying a CGM for insights into your body and the food you eat, here are some things to consider:
1. Would a CGM be useful to you?
Look at whether you have abnormal levels in the five parameters that give a glimpse of one's metabolic health. These can be obtained from a traditional health screening. They are: high blood pressure, high waist circumference, raised fasting sugar, low HDL cholesterol level and high triglyceride levels. If you have three or more, it will be beneficial to proceed to monitor your glucose levels with a CGM.
Dr Lam suggests,
2. Go pro to learn fast
Your first, or first few, experiences with a CGM should involve a health professional to help you through the steep learning curve, make sense of the data, and make appropriate diet and lifestyle adjustments to optimise health. Your preferred healthcare provider may be able to walk the CGM journey with you. Alternatively, qualified health coaches are also trained to help you understand your CGM experience.
3. Maximum value
Get the best bang for your buck and effort by logging what you are eating. It will help you identify what foods keep your body happy, or stress it out. Even better, log your exercise, sleep and moods with the CGM app.
Speaking of bucks, a CGM isn’t a cheap toy. It costs about $100 and is worn for two weeks.
But if it helps to steer me towards healthy choices that improve my health, it’s money I’d rather shell out for now, rather than wait for my health to break. And there’s never a convenient time to be ill!
The best experience I got out of wearing a CGM didn’t come from me. It came from an acquaintance who reached out to ask me about it when she saw my social media post on my CGM.
She’s diabetic and weary of her meds being constantly increased. She was ready to take charge of her health. This was what she shared some months later:
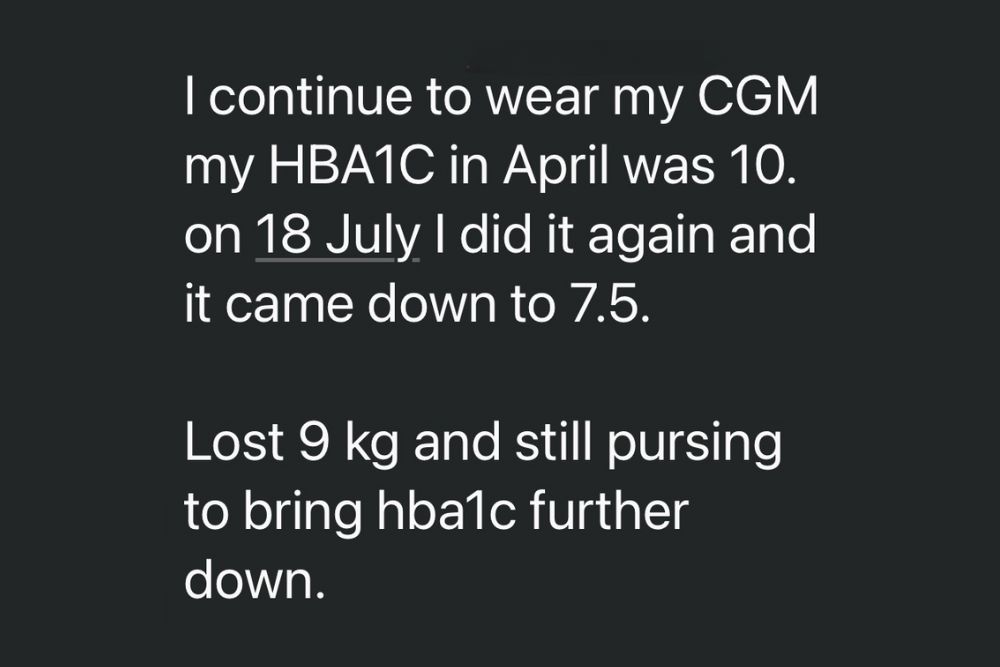
Knowing that sharing my CGM adventure helped someone towards better health was just priceless.
Kim Lee found her way to health coaching after becoming a brain feedback practitioner helping people optimise their brain function. Care of the body is care for the brain.
World Diabetes Day, 14 November 2024
‘Diabetes and Well-being’ is the theme for World Diabetes Day (WDD) 2024.
It focuses on individual health and stresses the need for communities to take action on this global issue.
WWD is celebrated on 14 November, the birthday of Sir Frederick Banting, discoverer of life-saving insulin in 1922.
WDD has been an annual awareness campaign by the International Diabetes Federation (IDF) and the World Health Organization (WHO) since 1991.
Find out more about WDD.






