
Glaucoma is called the “silent thief of sight” as the condition can cause blindness without a person being aware of it. Patients do not experience pain or symptoms till the condition is advanced.
Glaucoma is the leading cause of irreversible blindness in the world. 40% of blindness in Singapore is caused by glaucoma.

Glaucoma Screening
Early detection and treatment of glaucoma is important in preventing further damage and visual loss. If diagnosed early, it can be treated to prevent blindness.
Advertisement
The patient should see an eye specialist who will be able to determine if glaucoma is present and to assess its severity.
There is no cure for glaucoma but in most cases it can be successfully controlled with medical, laser or surgical treatment.
Patients will require long-term follow-up to ensure that the glaucoma control is adequate.
Types of glaucoma
Open-angle glaucoma
- Primary Open Angle Glaucoma
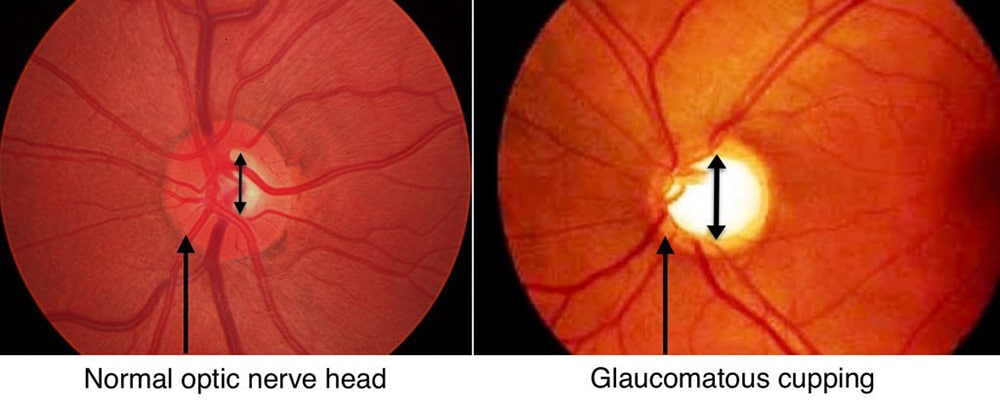
- Ocular hypertension (Glaucoma suspects) is classified as increased intraocular pressure without optic disc damage or visual field changes. Ocular hypertensives are glaucoma suspects and should be screened every year.
- Normal-Tension Glaucoma
Close-angle Glaucoma
- It occurs when there is obstruction of the flow of fluid through the drainage angle, which results in the increase in intraocular pressure, optic nerve damage and visual field loss. Blindness can result very quickly if untreated.
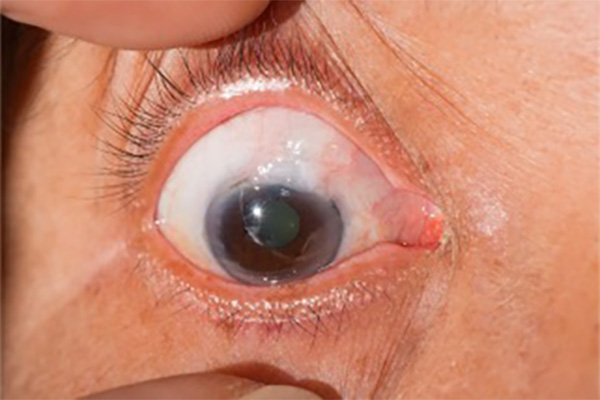
- Acute primary angle closure glaucoma is an ocular emergency. It commonly occurs in Asians. Symptoms include sudden eye pain and redness, blurred vision, haloes, nausea, vomiting and headaches. Blindness can result very quickly if untreated.
Secondary glaucoma
- It can be caused by trauma, inflammation and intraocular tumours.
Congenital glaucoma
- It occurs due to the underdevelopment of the drainage structures.
Risks factors
- Increasing age > 50 years old
- Positive family history of glaucoma
- High eye pressure
- Asian and African descent
- Females
- Systemic Diseases (Diabetes, Obstructive sleep apnoea, Cardiovascular diseases)
- Myopia or Hyperopia
- Trauma to the eye
- Previous eye surgery
- Use of steroids (cortisone medications)
Anyone above the age of 50 stands a chance of developing glaucoma and the risk increases as they age. Glaucoma is also strongly related to family history of the disease.
It is a myth that glaucoma is a very rare disease and only patients with medical issues such as diabetes will be diagnosed with glaucoma. Everyone above the age of 50 should have their eyes checked at least once by an ophthalmologist.
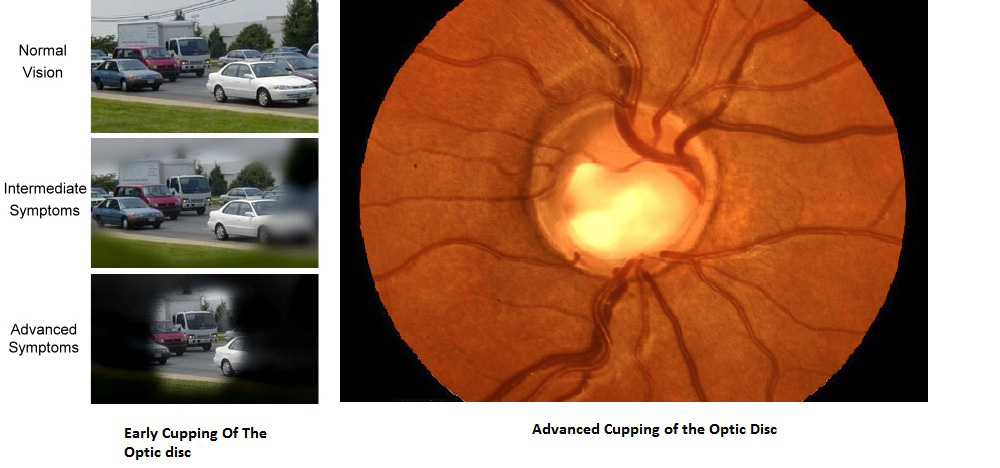
Effects of glaucoma
Patients who have early or moderate glaucoma do not experience any symptoms. It is a myth that patients with glaucoma always experience eye pain and headache.
Most patients have chronic progressive painless visual loss and only get diagnosed during a routine eye screening, as an incidental finding or during a visit to the optometrist.
Blurring of vision is usually present at a late stage when the visual loss is already irreversible. They are left with a tunnel vision and only the central vision remains.
Patients with advanced glaucoma have dim vision especially at night and may keep bumping into people or objects.
What can you do?
Following a healthy diet and regular exercise is beneficial to your overall health. There is no strong evidence about general diet or dietary supplements and its impact on glaucoma.
In general, a healthy diet rich in antioxidants would be beneficial to the eye but does not prevent glaucoma.
Too much screen time primarily affects younger children and increase their risk of myopia. It is not linked to increased risk of glaucoma.
Glaucoma management
The damaged caused by glaucoma cannot be reversed. But treatment and regular eye drops can slow the progression and help prevent vision loss.
Glaucoma is treated by lowering your eye pressure. Depending on the patient, your options may include prescription eye drops, oral medications, laser or surgery depending on the type and severity of glaucoma.
Regular Check-ups
Many elderly patients get frustrated with the regular visits to the ophthalmologists and stop going for follow-up treatments. When they return a few years later, they would have suffered severe visual loss, often too late for treatment or surgery.
Glaucoma is like diabetes mellitus and hypertension, it is a chronic disease and cannot be cured.
Patients who are on glaucoma eye drops need to be on regular follow-up with an ophthalmologist to ensure that the treatment is effective and they do not suffer from side effects (redness, itchiness, swelling of lids).
Defaulting treatment may cause irreversible and severe visual loss that will eventually lead to blindness.

Medications
The initial treatment of glaucoma often starts with prescription drops. The eyedrops help decrease the eye pressure by increasing drainage or decreasing the amount of fluid your eye makes.
Medications are the first line of treatment as they are safe and effective. Some patients can use multiple eye drops to control their eye pressure.

Laser treatment
Laser is an outpatient procedure done in the clinic. Laser treatment can be used to treat some types of glaucoma.
Laser iridotomy/ iridoplasty can be performed for angle closure glaucoma to relieve pupil blockages and helps widen the outflow drainage angle. It can prevent acute angle closure glaucoma.
Selective laser trabeculopasty is usually recommended for open angle glaucoma to increase outflow of the angle to decrease eye pressure. It is a safe procedure and can be repeated.
Surgery
Trabeculectomy is a filtering surgery performed by creating an opening on the eye for fluid inside the eye to be drained.
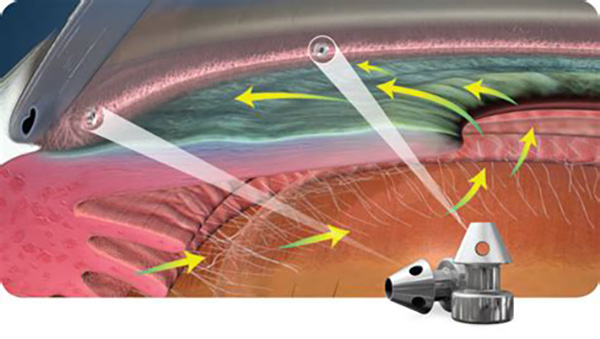
Tube-shunt surgery is a flexible glaucoma drainage device placed into the eye to drain excess fluid out of the eye.
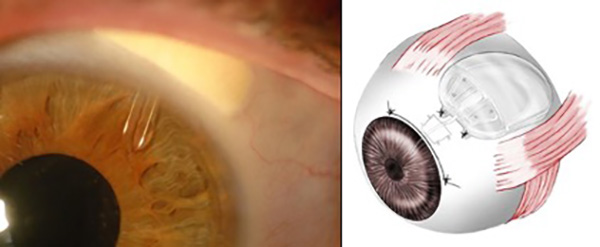
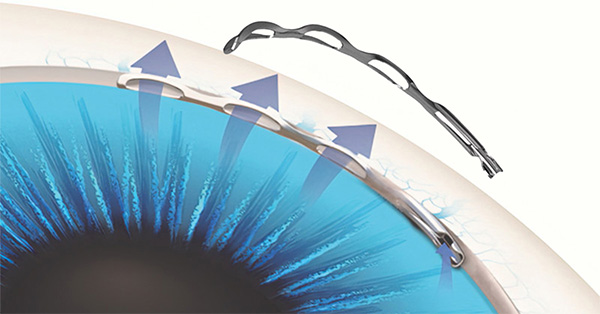
Minimally invasive glaucoma surgery – Minimally invasive glaucoma surgery has emerged as a new and effective treatment for patients with glaucoma. It is a microinvasive surgery with a very high safety profile and rapid post-operative recovery. It has greatly improved the quality of life for many glaucoma patients by reducing the number of glaucoma drops required by a patient after the procedure.
Istent inject allows increased drainage of fluid and lowers the intraocular pressure.
Hydrus microstent decreases outflow by 3 ways: Enhancing outflow; expand the eye’s natural fluid pathway; and reducing pressure reliably.
If you haven’t already been for an eye check-up, do so soon.
Dr Xu is a Consultant Ophthalmologist at Eye Specialist Clinic. She is one of only a few glaucoma specialists to have completed 3 advanced training fellowships.





